A decade of CAR-T cell therapy

Nina Notman looks at the revolutionary treatment already taking on cancer, now aiming for wider use
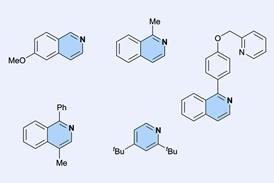
T cells are white blood cells with a vital role in our immune system. They host proteins called T cell receptors on their surface, and as the T cells circulate the body, these receptors recognise antigens on abnormal or infected cells. Then, depending on the type of T cells they are, they either destroy the damaged cells themselves or stimulate the other white blood cells around them to do so. A chimeric antigen receptor (CAR) is a genetically modified version of the T cell receptor that recognises specific antigens on a particular type of diseased cell.
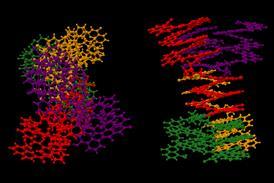
T cells are harvested from a patient’s blood by passing it through a machine that separates blood into its various components. The rest of the blood is then returned to the patient. The T cells are then sent to a centralised manufacturing facility where their genetic material is modified. A lentiviral or retroviral vector delivers the new genetic information to the T cell by attaching itself to the cell surface and injecting RNA into its cytoplasm. This genetic information is essentially the recipe needed to produce the CAR. The genetic recipe is then incorporated into the T cell’s genome, so the protein it codes for (the CAR) is synthesised and expressed on the surface of the T cell. The CAR-T cells are then multiplied, frozen and returned to the hospital for infusion back into the patient. Once in the body, the CAR-T cells seek out and destroy malignant cells that have expressed the target antigen on their surface.